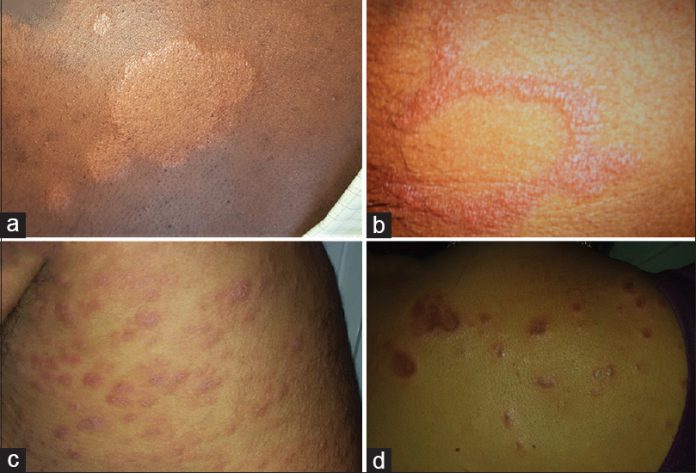
Masezza.com – The differential diagnosis of leprosy skin lesions is a complex process. The indeterminate form of leprosy must be distinguished from hypochromic and achromic lesions. Polymorphic and tuberculoid lesions may be mistaken for infectious sarcoid lesions. In addition, multibacillary lesions must be differentiated from those caused by secondary syphilis.
Leprosy affects the skin, peripheral nervous system and the eyes

The infection is a chronic and debilitating disease caused by an acid-fast bacterium called Mycobacterium leprae. Leprosy affects not only the skin, but also the peripheral nervous system and eyes. It develops slowly over time, ranging from six months to 40 years. Leprosy causes skin lesions, deformities, and pain. Typically, affected parts of the body are cooler than the rest. Symptoms are disfiguring and can affect any part of the body, including the eyes, nose, upper respiratory tract mucous membranes, eye, muscles, bone, and testes. Infection is contagious through nasal secretions, droplets, and direct contact, but is rarely spread by skin to skin.
After leprosy infection, the symptoms may be noticeable one to three years later. Leprosy involves the skin and peripheral nerves, causing numbness and weakness in affected areas. In tuberculoid leprosy, central hypopigmented macules may be present. The nerves are damaged in the underlying tissues, making the areas affected numb. Patients may also experience palpable enlarged peripheral nerves.
The only medicine is prevention

The immune response in leprosy is complicated by the inability to produce sufficient antibodies. It can take several years for the immune system to develop a robust response. Ultimately, the infection must be stopped to prevent the spread of the disease. Vaccines and antivirals may be helpful, but the only cure is prevention. The only way to prevent leprosy skin lesions is to control the infectious process.
Treatment of leprosy skin lesions is possible if the lepromatous person can undergo MDT within 72 hours. However, leprosy cannot be spread by sexual contact, and antibiotics are necessary for effective treatment. Patients should be encouraged to participate in normal social life. Although leprosy is a chronic bacterial infection, it can be cured with antibiotics and anti-fungal drugs.
The granulomatous spectrum reflects the immune response .

Clinically, skin lesions of leprosy may appear as a spectrum of granulomatous and tuberculoid types. The granulomatous spectrum reflects the immune response. The tuberculoid spectrum, however, has no bacilli. The granulomatous spectrum, on the other hand, displays the presence of bacilli disseminated throughout the skin.
Macrophages have two major roles in the immune response in leprosy. They are either M1 or M2, and their function depends on their cytokine profile. In addition, macrophages may express other factors. Some of these factors are responsible for leprosy skin lesions. They may also affect the synthesis of certain cytokines. This is why it is essential to understand the immune responses in leprosy skin lesions.
Cytokine pattern becomes dominant during the reversal reaction phase

The immune response to an invading pathogen is critical for the host’s defense against the pathogen. Leprosy skin lesions in tuberculoid and lepromatous lesions exhibit a Th1 cytokine pattern. Interestingly, the Th2 cytokine pattern is expressed in lepromatous lesions as well. In some patients, this cytokine pattern becomes predominant during the reversal reaction phase, which occurs when the patient upgrades from the L-lep pole to the T-lep pole.
The apoptosis of macrophages in leprosy skin lesions correlates with the induction of anti-inflammatory mediators. Other pro-inflammatory cytokines, including TNF, contribute to the apoptotic process of Schwann cells. The immune system responds by producing a cytokine, TNF. This reaction is associated with the pathogenesis of leprosy skin lesions.